Fibromyalgia
What is Fibromyalgia?
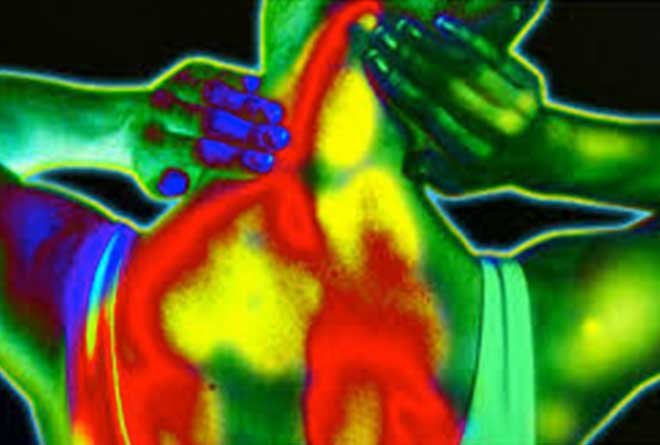
FMS (Fibromyalgia Syndrome) is a widespread pain and fatigue syndrome without a known cause. The earliest description of FMS in the medical literature dates back to 1869 when the Physician George Beard described a syndrome he named Neurasthenia, and later in 1904 a Neurologist, William Gower coined the term “Fibrositis”. In 1976, the name was changed to Fibomyalgia which means pain in the muscles, ligaments, and tendons. Most patients with Fibromyalgia complain of hurting all over or “from head to toe”. The neck and back, hips and shoulders are typically prominent complaints. They will also complain of burning sensations, numbness, dry eyes, dry mouth, temperature sensitivity and feeling cold, headaches, fatigue, poor sleep, dizziness, abdominal and bladder problems, sensitivities to medications, restless legs, jaw discomfort, and difficulties with mood, memory and constipation.
How is FMS Diagnosed?
The official criteria was developed by the American Academy of Rheumatology, and includes pain in the left and right sides of the body and upper and lower half of the body for at least 3 months. There must also be at least 11 of 18 anatomically specific “tender points”. Laboratory tests may be unremarkable but hormone and autoimmune tests sometimes reveal abnormalities. Overnight sleep studies are commonly ordered now as over 50% of patients are found to have sleep disordered breathing, many have periodic limb movement disorder and most have problems with little or no deep sleep. Most patients with FMS have a problem with their deep sleep known as “Alpha/Delta” sleep, a persistence of wake-like brain patterns throughout the night, but many sleep labs do not routinely screen for this unfortunately. MRIs might be ordered to rule out other conditions that can affect the brain and spinal cord.
Symptoms and Associated Syndromes
- Pain: though the whole body can hurt at times, the spine, neck, shoulder hips and knees tend to be the most prominent areas involved. The pains can come and go and move around making it difficult for the patient and doctor to understand what is happening. Patients can also have tingling, burning types of symptoms in their hands and feet or other parts of their bodies. Anti- inflammatories usually do not provide significant relief and even strong narcotic analgesics provide little in the way of pain relief, and so are not recommended.
- Fatigue: fatigue can be mild or disabling. This can be “brain fatigue” where there is difficulty with memory, attention, concentration, and multitasking, commonly referred to as “fibrofog”. The fatigue will typically manifest as the feeling of having no energy or being unable to work, exercise, or sometimes even move. Many patients will meet official criteria for Chronic Fatigue Syndrome.
- Sleep: Patients complain of waking up feeling they haven’t slept at all and not getting deep sleep, , referred to as “non-restorative sleep”. Even if they do get deep sleep, known as “Delta sleep”, their brain waves appear as if they are still awake, called “Alpha Wave Intrusion”. Insomnia, Sleep Apnea, and Restless Legs are all common, can be identified by sleep studies and are amenable to treatment.
- Irritable Bowel Syndrome: Anywhere from 40% to 70% of patients with FMS will meet the criteria for Irritable Bowel Syndrome (IBS). Symptoms can include constipation, diarrhea, abdominal pain, gas, nausea, and bloating.
- Irritable Bladder: Many patients with FMS will also complain of difficulty with frequent need to urinate, or sense of urgency, and even in some cases urinary incontinence, sometimes diagnosed as interstitial cystitis.
- Tension Headache and Migraine: Many FMS patients suffer with recurrent headaches that can have the characteristics of tension headaches or of migraine headaches.
- Multiple Chemical Sensitivity: A third of patients with FMS are sensitive to odors and very intolerant of many medications and report that they “get every side effect”, and so typically cannot tolerate pharmaceuticals.
- Primary Dysmennorhea: Painful and irregular periods can be experienced with many female patients. This has lead to increase use of birth control pill to help control the symptoms. Some patients undergo total hysterectomies leaving them without any ovarian hormones which makes hormonal balance more challenging.
- Temporomandibular Joint Dysfunction: Many FMS patients have tremendous jaw and face pain.
- Myofascial Pain Syndrome: The majority of patients have pain in the muscles, joints, tendons, and ligaments. Morning stiffness is commonly reported in FMS patients.
- GENETICS: A family history is seen in one third of patients. Research is looking at the COMT gene which plays a role in serotonin regulation, the autonomic system, and pain control.
- NEUROCHEMISTRY: The best documented abnormality in FMS is low serotonin levels in the spinal fluid which could impair the nervous system ability to control pain signals. Substance P is the major pain signaller and studies have shown it is elevated 300%. Pain in FMS is not caused by inflammation, but a signal processing error that causes pain amplification within the Central Nervous System.
- HORMONES: Abnormalities have been shown in growth hormone, thyroid hormones and antibodies, cortisol , estrogen, progesterone, and testosterone. Early childhood trauma or turbulence, whiplash injuries, extremely stressful events, and even infections have been associated with the development of FMS by disrupting regulation of the hypothalamic pituitary-adrenal axis.
- SLEEP: Deep sleep or slow wave sleep is responsible for tissue repair, immune system regulation, hormonal and neurochemical regulation. Disturbed deep sleep (Alpha-Delta Sleep), which is seen in the majority of patients, is associated with many of the neurochemical and hormonal problems in FMS and is consequently a major focus in current research and treatment.
What is the cause of Fibromyalgia?
The ultimate cause of FMS is still a mystery, but there is a lot that is now known about this condition...
How do we treat Fibromyalgia?
Reduction of pain is a primary goal and medications that boost serotonin and norepinepherine such as duloxetine and milnaciprin which are both now FDA approved for the treatment of FMS. These SNRI's can occasionally cause nausea, sleep problems, sweating, and decreased libido. Pregabalin, which is also FDA approved, has been studied and shown to be effective for treatment of pain but can cause swelling, and weight gain, as well as somnolence. A few patients can respond to medications that work through dopamine such as Wellbutrin or Mirapex.
Decreasing Substance P with agents like Tizanidine can also be helpful for pain and muscle spasm and may help sleep. Narcotic agents are thought to be a last choice but the pseudo-narcotic Tramadol can be safe and effective. Experimental medications that improve deep sleep, such as Sodium Oxybate, are currently under investigation but other sleep aids are frequently used.
Hormonal manipulation may provide benefit in some patients. Stimulants can be useful for cognitive impairment and fatigue. Beta-blockers, though they can interfere with sleep and mood, can be helpful for autonomic dysfunction which is commonly seen in FMS. Gaufenesin, which had been used frequently in the past, is now no longer considered a mainstay of therapy as it has not been shown to be helpful in randomized-blinded trials.
A healthy diet low in refined sugar may help some patients. Gluten sensitivity or allergy is also seen in some patients and can mimic many symptoms of FMS. Stretching, low impact aerobic exercise, and aquatic therapy can also be helpful. Organized stress reduction is critical, meditation and yoga have been found to be beneficial
For more information or to schedule an appointment, please call 912.298.6646
New Patient appointments require a referral from your Physician. Please contact your Physician's office and have them fax a referral to 912.298.6622
